Amity’s News!
Outsourcing coding and clinical documentation review to dedicated professionals is one of the most effective strategies to strengthen and enhance documentation from regulatory, payment, and legal perspectives.
- ICD – 10 Coding
- OASIS Review + ICD – 10 coding
- OASIS Review + POC (Plan of Care) Review
- OASIS Review + ICD – 10 Coding + POC (Plan of Care) Review
- Episodic documentation review
- Quality Trends Analysis and QAPI Development
For more information or a free trial, please contact us at 303-690-2749 or email at ig@amityhealthcaregroup.com
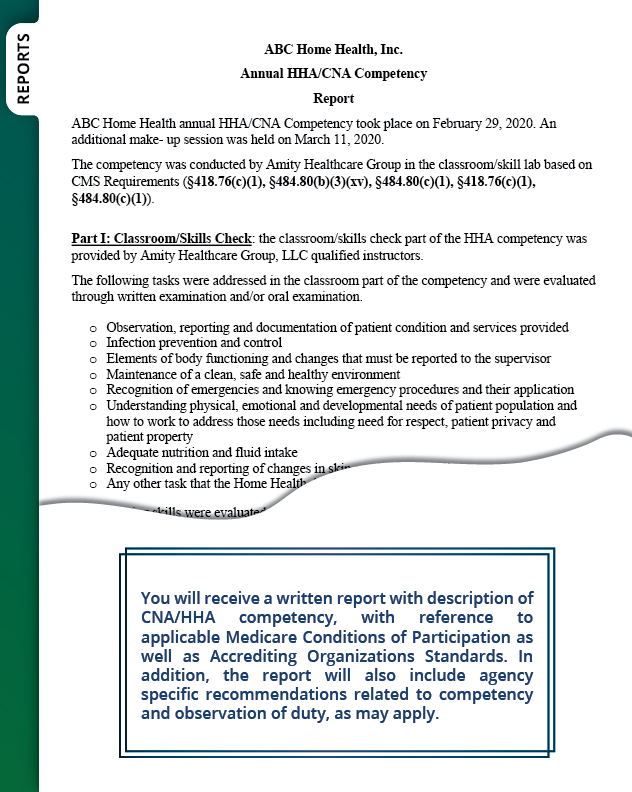
Home Health Skilled Nursing Competency Program

The “virtual” Skilled Nursing Competency program offered by Amity Healthcare Group, LLC is designed to assist agencies in meeting initial onboarding and/or annual competency requirements for Registered Nurses (RNs) and Licensed Practical/ Vocational Nurses (LPN/LVNs) in the home health care setting.
![]()
This comprehensive program serves as a robust introductory foundation to nurses new to the home health setting as well as an excellent “refresher” for experienced home health nursing staff.
Please note that our skilled nursing competency program is certified by Accreditation Commission for Health Care (ACHC) (learn more here).
For more information, questions, or registration for Amity’s home health skilled nursing competency program, please go to https://amityhealthcaregroup.
OASIS -E Corner

In this issue, we would like to address the question about OASIS Item D0150- Patient Mood Interview:
![]()
Question:
Please clarify when the entire Patient Mood Interview should be completed for D0150 -Patient Mood Interview (PHQ-2 to 9). The instruction in the OASIS-E Guidance Manual appears to conflict with the language in the D0150 item.
Answer:
Please use instruction found in the Response-Specific Instructions for D0150 in the OASIS-E Guidance Manual. Whether or not further evaluation of a patient’s mood is needed depends on the patient’s responses to the PHQ-2 (D0150A and D0150B). If both D0150A1 and D0150B1 are coded 9, OR, both D0150A2 and D0150B2 are coded 0 or 1, END the PHQ interview; otherwise continue.
For all other scenarios proceed to ask the remaining seven questions (D0150C to D0150I) of the PHQ-9 and complete D0160, Total Severity Score.
NATIONAL NEWS

CMS Ends COVID-19 Vaccination Requirements
![]()
As expected after the memo that was issued by the Centers for Medicare & Medicaid Services (CMS) on May, 2023, CMS has issued a final rule ending the COVID-19 vaccination requirements for health care providers.
The rule covers all participating providers, including home health, and withdraws the regulations in the IFC “Omnibus COVID-19 Health Care Staff Vaccination” published in the November 5, 2021, Federal Register. The rule removes in its entirety the standards for “COVID–19 Vaccination of Home Health Agency staff” §484.70(d) from the conditions of participation.
Home health: § 484.70(d)
§ 484.70(d) Standard: COVID–19 Vaccination of Home Health Agency staff. The home health agency (HHA) must develop and implement policies and procedures to ensure that all staff are fully vaccinated for COVID–19. For purposes of this section, staff are considered fully vaccinated if it has been 2 weeks or more since they completed a primary vaccination series for COVID–19. The completion of a primary vaccination series for COVID–19 is defined here as the administration of a single-dose vaccine, or the administration of all required doses of a multi-dose vaccine.
This final rule is set to be published in the Federal Register on June 5, 2023, and will become effective 60 days after it is posted to the register (August 4, 2023).
Continued compliance with the COVID-19 vaccination rules will be assessed until the time the final rule becomes effective to end the requirement.

Ending of the COVID-19 PHE Waivers & Flexibilities
As the Public Health Emergency (PHE) expired on May 11, 2023, providers continue to have questions about waivers and flexibilities issued during the PHE and their status.
![]()
National Association for Home Care and Hospice developed a reference TOOL to address ending of the COVID-19 PHE waivers/flexibilities, including the status of each waiver/flexibility and an associated compliance date.
Please note that in addition to the information included in the tool, CMS issued additional clarification related to OASIS completion and submission and its impact on payment as follows:
The extension of the five-day completion requirement for the comprehensive assessment waiver at SOC would be based on the M0030 – Start of Care (SOC) date. For example, if the M0030 – SOC date is on or before 5/11/23, the five-day extension waiver is in effect. However, If the M0030 – SOC date is on or after 5/12/23 or later, the five-day extension waiver has expired.
What concerns the waiving of the 30-day OASIS submission requirement, this would be based on the M0090 – Date Assessment Completed. For example, if an assessment’s M0090 date is on or before 5/11/23, the 30-day submission requirement for that assessment would be waived. If an assessment’s M0090 date is on or after 5/12/23 or later, the 30-day submission requirement is in effect.
Revised Masking Guidance

As waivers, flexibilities, and rules related to COVID-19 Public Health Emergency and its expiration are being revised, the Centers for Disease Prevention and Control (CDC) has also issued a revision to the guidance for Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic.
The guidance applies to all health care settings and provides a framework to implement infection prevention and control practices based on their individual circumstances.
In making a decision about a broad use of masking in the healthcare setting, CDC recommends taking several considerations into the account as follows:
- The types of patients you care for
- Healthcare settings may develop their interventions based on the population they serve. For example, home health agencies might consider establishing policies for masking when caring for patients with a high risk for contracting infectious diseases/patients who are immunocompromised.
- Type of available data/metrics to assist with decision-making regarding broad masking
- Input from stakeholders
- Reviewing of the plans/interventions with stakeholders including patients and healthcare personnel can help an organization to identify appropriate masking practices.
Renewed ABN Form

Just a reminder that the Advanced Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, and form instructions have been approved by the Office of Management and Budget for renewal.
![]()
The use of the renewed form with the expiration date of 01/31/2026 will be mandatory on 6/30/23.
Providers may continue to use the ABN form with the expiration date of 6/30/23 until the renewed form becomes mandatory on 6/30/23. The ABN form and instructions may be found here in the downloads section.
6th Annual Home Health Value Based Purchasing Report Released

The 6th annual HHVBP report is now available for review.
The Report focuses on the experience of home health patients and agencies through 2021, the fourth and final year that eligible agencies in the nine original Home Health Value Based Purchasing (HHVBP) states received an adjustment to their Medicare payment amounts under the Home Health Prospective Payment System (HH PPS).
Several of the key findings include:
- Agency Total Performance Scores are higher in each of the six years of the original model.
- Cumulative decline of $1.38 billion in overall Medicare spending for FFS beneficiaries receiving home health services during 2016-2021.
- Reductions in unplanned hospitalizations and use of skilled nursing facilities.
- Increase in outpatient emergency department use accompanied by a decrease in emergency department use leading to an inpatient admission.
- Gains in quality of care include greater improvements in functional outcomes.
- Increase in shift of skilled nursing and therapy visits to early weeks of home health episode among HHVBP agencies.
HCS Home Care/Hospice Salary & Benefits Studies Underway

Hospital & Healthcare Compensation Service (HCS) have announced the 2023‑2024 Home Care and Hospice Salary & Benefits studies are now underway.
The reports offer a valuable resource for comprehensive marketplace data for home health and hospice agencies. Last year’s reports contained data from 867 home health agencies and 674 hospice agencies.
Both studies include questions on staffing issues, nursing vacancy and turnover rates, and sign-on bonuses used by agencies to attract new employees. The results cover job data by salary, hourly, and per visit rates with job data breakouts by revenue size, region, state, etc. The Home Care results cover marketplace data for 59 jobs; the Hospice results cover 62 jobs. Regional data for 21 fringe benefits, planned salary increases, productivity, caseload, and shift differential data are also covered.
If you would like to participate in the HCS Home Care or Hospice Salary & Benefits Study, please follow the instructions below:
- Download the questionnaire from the HCS website: hhcsinc.com
- Select either the single site or multi-site questionnaire for the Home Care or Hospice study
- Email Rosanne Zabka, HCS, rzabka@hhcsinc.com to confirm your planned participation
- Email your completed questionnaire to HCS by August 7th
There is no cost to participate. Participants save over 50% off the Report price.
Please note that all individual data will be kept strictly confidential. Study results are reported as aggregated percentiles per job. No information will be released to any person or organization which will identify individual participants.
| Participant Pricing | Home Care | Hospice |
|---|---|---|
| Prepaid Rate (due by 8/31/23) | $185 | $160 |
| Billed Rate | $205 | $180 |
| Non-participant Rate | $375 | $325 |
The COVID-19 Public Health Emergency (PHE)
The COVID-19 Public Health Emergency (PHE) ended on May 11, 2023. To learn more about Colorado and COVID-19 Emergency Federal Flexibilities that have been made permanent and those that are changing, refer to the Overview of COVID-19 Emergency Federal Flexibilities – Colorado Medicaid section on the End of the Public Health Emergency web page. The web page features a chart of what flexibilities were requested, what was used, what policy changes were made permanent and what will be changing at the conclusion of the PHE.
As you are reviewing the updates to the Colorado waivers and flexibilities, please note specific changes to telemedicine requirements post Public Health Emergency (PHE). The following is a list of notable changes related to telemedicine that may impact home health agencies.
Services that have been made permanent:
Health First Colorado has expanded the list of providers eligible to deliver telemedicine services to include physical therapists, occupational therapists, home health providers, hospice and pediatric behavioral health providers.
Home health agency services and therapies, hospice, and pediatric behavioral treatment may be provided via telephone-only.
[please note that provision of care via telemedicine/phone only must be reasonable for patient’s needs and plan of care and may not be appropriate when direct observation is required]
Other changes:
All consent for telemedicine services could be verbal during the PHE. Providers must obtain written consent prior to the first visit post-PHE, as described in the Waiving the Face-to-Face Requirement & Required Disclosure Statements section of the Telemedicine Billing Manual.
The written consent should include the following verbiage:
[prior to treating the member through telemedicine for the first time, the provider must furnish each member with all of the following written statements, which must be signed (electronic signatures will be accepted) by the member or the member’s legal representative]:
- The member retains the option to refuse the delivery of health care services via telemedicine at any time without affecting the member’s right to future care or treatment and without risking the loss or withdrawal of any program benefits to which the member would otherwise be entitled.
- All applicable confidentiality protections shall apply to the services.
- The members shall have access to all medical information resulting from the telemedicine services as provided by applicable law for member access to his or her medical records. [C. R. S. 2018, 25.5-5-320 (4)].
Fiscal Year 2023-2024 Provider Rate Adjustments

Health First Colorado (Colorado’s Medicaid program) across-the-board (ATB) provider rate increases were approved during the 2022 legislative session and are effective for dates of service beginning July 1, 2023. All rate adjustments are subject to Centers for Medicare & Medicaid Services (CMS) approval prior to implementation.
![]()
The fee schedules located on the Provider Rates and Fee Schedule web page will be updated to reflect the approved 3.0% ATB rate increases. Rates will be updated in the Colorado interChange for dates of service beginning July 1, 2023
Amity’s newsletters will be archived on Amity’s Healthcare Group website at https://amityhealthcaregroup.
Please do not hesitate to reach out for any assistance or questions via email, phone, or website at https://amityhealthcaregroup.
If you wish to forward this email to your colleague or friend, please feel free to do so. If you received this message as a forward, we invite you to subscribe to our communications at https://amityhealthcaregroup.
Thank you,
Irina Gorovaya, RN BSN, MBA
Amity Healthcare Group, LLC
Home Health Consulting, Education and Outsourcing Services
720-353-7249 (cell) 303-690-2749 (office) 720-398-6200 (fax)
www.amityhealthcaregroup.com







Confidentiality Notice:
The information contained in this message is privileged and confidential information intended for the use of the individual or entity named above.Copyright © 2022 Amity Healthcare Group, All rights reserved.
You are receiving this email because you opted in at our website
Amity Healthcare Group
5600 S. Quebec St Suite 310-A
Greewood Village, CO 8011