Amity’s News!
Attention Colorado HCBS Providers and Direct Care Workers!
Amity Healthcare Group is offering free specialized dementia training courses for Colorado HCBS providers/direct care workers.
Providers will be able to select from the following courses:
- The Alzheimer’s and Dementia Caregiving at Home (available on Mondays and Wednesdays)
- Creating Safe Home Environment for People Living with Dementia and Alzheimer’s Disease (available on Fridays)
To register for your free course, please go HERE
ACHC Product Certification- Emergency Preparedness Plan
We are also excited to announce that Amity Healthcare Group received additional ACHC product certification for Emergency Preparedness Plan for home health and home care providers.
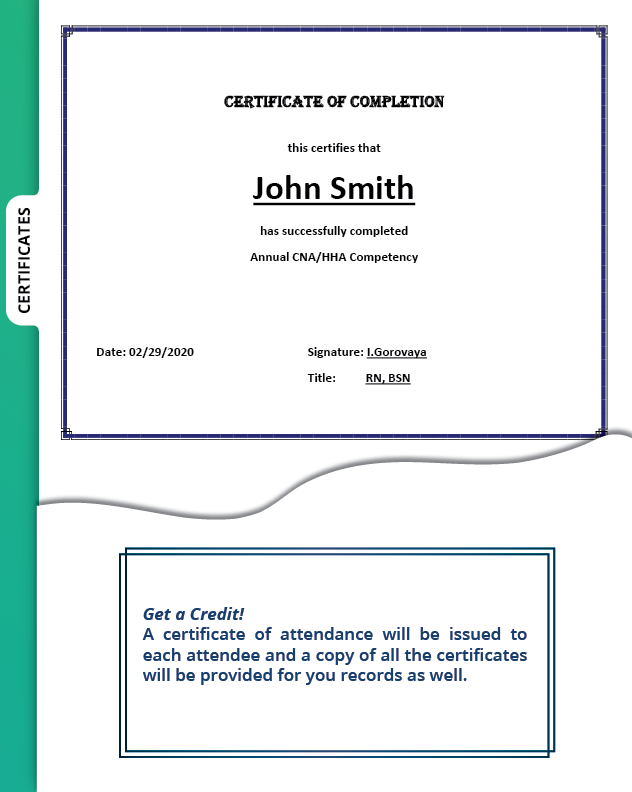
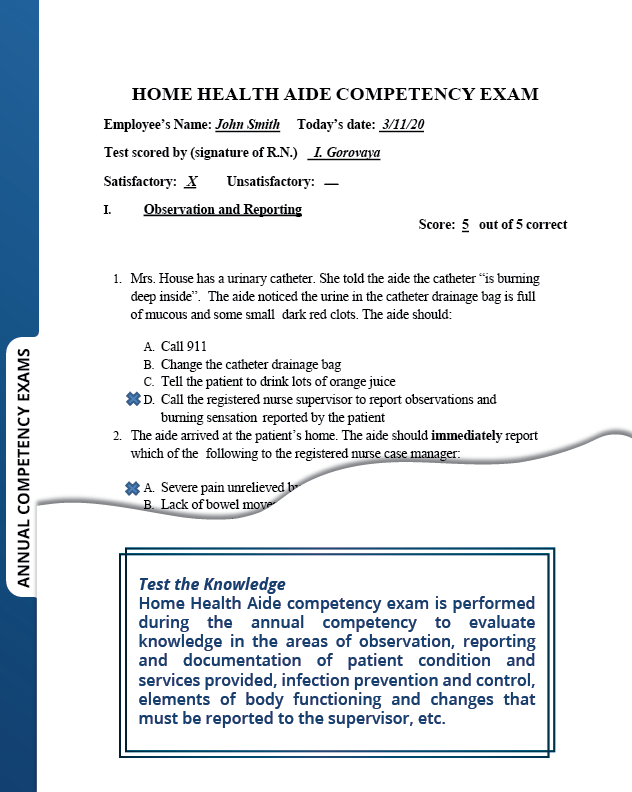
We now offer the following ACHC certified products for home health and home care agencies:
- Home Health and Home Care admission packet
- Home Health and Home Care QAPI program
- Home Health and Home Care Emergency Preparedness Plan
- Home Health Skilled Nursing Competency Program
ORDER YOUR COPY TODAY!
For more information about our CHAP and ACHC certified products, please call 303-690-2749 or email ig@amityhealthcaregroup.com.
Please also visit our website at https://amityhealthcaregroup.
OASIS -E Corner
Discharge OASIS Guidance:
Discharge requires a visit to complete the assessment. In the case of an unplanned discharge, CMS still requires the DC OASIS to be based on an assessment.
Please see guidance for the following items when completing an unplanned/non-visit discharge:
B1300 Health Literacy: the question in this item must be asked of the patient and no one else. The clinician cannot make assumptions. If the patient cannot be asked, the best response may be ‘8 Patient unable to respond.’
C0100‐C0500 BIMS C0100 can be answered based on information documented in the last visits. However, the actual BIMS (Brief Interview for Mental Status) item requires patient performance. Was there a BIMS used with the patient at the last visit (within the past 5 days)? A dash indicates no information. Unless you can get the patient to respond to the screening, you will need to respond with dashes. C0500 will be scored with a dash.
C1310 CAM: this item requires observation of the patient. It is not an interview item. Unless there is enough relevant information in the documentation from the last visits (within the past 5 days), this entire item will be dashed.
D0150‐D0160 Patient Mood Interview: the PHQ2‐9 requires interview of the patient. If a patient interview is not possible, then dashes are appropriate in column 1. A dash is never appropriate in column 2. If the interview is not conducted, score D0160 as 99. A dash is not appropriate in D0160.
D0700 Social Isolation: the question in this item must be asked of the patient and no one else. The clinician cannot make assumptions. If the patient cannot be asked, the best response may be ‘8 Patient unable to respond.”
J0510‐J0530 Pain Interview: the timeframe for this item is ‘in the last 5 days.’ The patient should have been asked these questions within the last 5 days. Any pain assessments should include the frequency of pain interference with activity. If unable to ascertain the correct responses and no visits within past 5 days, ‘8‐Unable to answer’ is the only valid choice as a dash is not appropriate.
For additional guidance on unplanned discharges without a visit, please see the following OASIS Q&As: https://www.cms.gov/Medicare/
NATIONAL NEWS
CMS Releases FAQ on CMS Waivers and Flexibilities and the End of PHE
On April 27, 2023, the Centers for Medicare & Medicaid Services (CMS) issued FAQs on CMS Waivers, Flexibilities, and the End of the COVID-19 PHE.
These FAQs will help you prepare for the expiration of the COVID-19 PHE and are relevant for all CMS programs; including, Medicare, Medicaid, the Children’s Health Insurance Program (CHIP), and private insurance.
OCR Announces Expiration of HIPAA Enforcement Discretion Issued in Response to COVID-19
As you may remember, in 2020 and 2021, Office for Civil Rights (OCR) published several Notifications of Enforcement Discretion in the Federal Register regarding how the Privacy, Security, Breach Notification, and Enforcement Rules (“HIPAA Rules”) would be applied to certain violations during the COVID-19 nationwide public health emergency.
One of these notifications (please see below) directly impacted home health industry and allowed covered health care providers to use popular applications that allow for video chats, including Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, Zoom, or Skype, to provide telehealth services without risk that OCR might seek to impose a penalty for noncompliance with the HIPAA Rules.
OCR Notification: Enforcement Discretion for Telehealth Remote Communications During the COVID–19 Nationwide Public Health Emergency – PDF
Recently, OCR issued a Federal Register notice that the enforcement discretion of certain rules under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the Health Information Technology for Economic and Clinical Health (HITECH) Act will expire on May 11, 2023 with the end of the COVID-19 public health emergency.
However, on April 11, OCR announced that they are providing a 90-calendar day transition period for covered health care providers to come into compliance with the HIPAA Rules with respect to their provision of telehealth. The transition period will be in effect beginning on May 12, 2023, and will expire at 11:59 p.m. on August 9, 2023. OCR will continue to exercise its enforcement discretion and will not impose penalties on covered health care providers for noncompliance with the HIPAA Rules that occurs in connection with the good faith provision of telehealth during the 90-calendar day transition period. The 90-day period will allow additional time for providers to transition from using non- HIPAA compliant telehealth technologies that have been permitted during the COVID-19 PHE to HIPPA secure solutions.
In the original notice for the telehealth remote communication enforcement discretion, the OCR provided a list of commonly used technologies, that are HIPAA compliant and will enter into HIPAA business associate agreements (BAAs).
Advance Beneficiary Notice of Noncoverage: Form Renewal
The Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, and form instructions have been approved by the Office of Management and Budget (OMB) for renewal. The use of the renewed form with the expiration date of 01/31/2026 will be mandatory on 6/30/23. You may continue to use the ABN form with the expiration date of 6/30/23 until the renewed form (expiration date 01/31/2026) becomes mandatory on 6/30/23. The ABN form and instructions may be found below in the downloads section.
The revised form can be found here in the downloads section.
CMS Finalizes CY 2024 Medicare Advantage Rule
On April 5, 2023, the Centers for Medicare & Medicaid Services (CMS) issued a final rule: Contract Year 2024 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly that implements several provisions from a December 27, 2022 proposed rule aimed at protecting beneficiaries enrolled in Medicare Advantage (MA) plans.
The National Association for Home Care and Hospice provided the following summary of the CY Medicare Advantage Rule provisions most important for home health providers:
Coverage Criteria
- Requires that MA plans must comply with national coverage determinations (NCD), local coverage determinations (LCD), and general coverage and benefit conditions included in Traditional Medicare regulations.
- When coverage criteria are not fully established, MA organizations may create internal coverage criteria based on current evidence in widely used treatment guidelines or clinical literature made publicly available to CMS, enrollees, and providers.
Prior Authorization and Utilization Management
- Limit the use of prior authorization processes only to confirm the presence of diagnoses or other medical criteria that are the basis for coverage determinations for the specific item or service
- Requiring that a granted prior authorization approval remains valid for as long as medically necessary.
- MA plans must establish a Utilization Management Committee to review all utilization management, including prior authorization, policies annually and ensure they are consistent with the coverage requirements.
- Requiring denials of coverage based on medical necessity be reviewed by health care professionals with relevant expertise before a denial can be issued.
Marketing
- Notifying enrollees annually, in writing, of the ability to opt out of phone calls regarding MA and Part D plan business.
- Requiring agents to explain the effect of an enrollee’s enrollment choice on their current coverage whenever the enrollee makes an enrollment decision.
- Simplifying plan comparisons by requiring medical benefits be in a specific order and listed at the top of a plan’s Summary of Benefits.
- Limiting the time that a sales agent can call a potential enrollee to no more than 12 months following the date that the enrollee first asked for information.
- Limiting the requirement to record calls between third-party marketing organizations (TPMOs) and beneficiaries to marketing (sales) and enrollment calls.
- Prohibiting a marketing event from occurring within 12 hours of an educational event at the same location.
- Clarify that the prohibition on door-to-door contact without a prior appointment still applies after collection of a business reply card or scope of appointment card.
- Prohibiting marketing of benefits in a service area where those benefits are not available,
- Prohibit advertisements if they do not mention a specific plan name,
- Prohibit the use of the Medicare name, CMS logo, and products or information issued by the Federal Government, including the Medicare card in advertisements , in a misleading way.
- Strengthens accountability for plans to monitor agent and broker activity.
- Prohibits advertising inaccurate cost savings.
Health Equity
- Establishing a health equity index in the Star Ratings program will reward Medicare Advantage and Medicare Part D plans that provide excellent care for underserved populations.
COLORADO NEWS
Colorado Direct Care Worker Appreciation Week
In recognition of Colorado’s 60,000 direct care workers, Gov. Jared Polis declared April 2 to April 8, 2023, as direct care worker appreciation week. Direct care workers provide care and assistance with activities of daily living to more than 70,000 people who receive long-term services and support in their homes, host homes, group homes, assisted living residences, and nursing homes.
Direct Care Worker Support Resources
As we are talking about staff appreciation, it is important to take into consideration that it is vital for the organizations to make the welfare of all direct care personnel to be central part of the organization by creating a culture of caring for both clients/patients and professional caregivers.
The State of Colorado Health Care Workforce Resilience & Retention Initiative’s CO-CARES Team (Colorado Alliance for Resilient & Equitable Systems for the Health Care Workforce) is offering additional recourses for organizations/providers to explore solutions to prevent staff burnout and develop a supportive and meaningful work environment that brings back joy in work.
Join CO-CARES to dive into the Joy In Work Toolkit created by the National Association of County and City Health Officials. This free webinar series will help teams and change leaders in the healthcare sector to build healthy, meaningful work environments.
During the webinar series, CO-CARES will identify barriers to joy in work that lead to staff turnover and burnout and explore strategies to address them. The series will run from May through October 2023, with one live webinar per month with two days/times to choose from. To learn more about the Institute for Healthcare Improvement and their framework for Joy in Work, watch here!
Signing up for the Joy in Work webinar will give you access to:
- Joy in Work Cohort on the Qooper platform where you can network, participate in discussions, give and receive peer support, and ask questions.
- Monthly newsletter.
- Coffee chats.
- Supplemental materials to assist organizations in understanding and implementing the program.
- Webinars to watch and re-watch as needed on your own time.
Find more information and sign up for the Joy in Work webinar series. If you have any questions, email COCARES: cdphe_healthcareworkersupport@
In addition, CO-CARES Team is offering virtual Psychological First Aid (PFA) training via the CoTrain portal. The course will address the ability to respond adaptively to stress, keep people calm, and support co-workers, patients, and family members who are experiencing stress and uncertainty is integral to the well-being of health care workers and caregivers. This training will explore tools to support and assist others’ adaptive functioning during times of stress, as well as basic coping strategies. PFA training is an evidence-informed approach built on the concept of human resilience and tailored to help better recognize, understand, and manage symptoms of psychological distress. It’s a way to give emotional support to people of any age, ethnic and cultural heritage, and social and economic background.
The training is available on the following dates:
- May 8th- 1:00 – 3:00 p.m.
- May 24th- 8:30 – 10:30 a.m.
Register in Co.Train (Course ID: 1020567)
This is a live, certificate training course (certificate issued after completion of training).
Please contact Danielle Aguilar for any accommodation requests or questions
Or the CO-CARES team:
CDPHE HealthcareWorkerSupport – CDPHE
Amity’s newsletters will be archived on Amity’s Healthcare Group website at https://amityhealthcaregroup.
Please do not hesitate to reach out for any assistance or questions via email, phone, or website at https://amityhealthcaregroup.
If you wish to forward this email to your colleague or friend, please feel free to do so. If you received this message as a forward, we invite you to subscribe to our communications at https://amityhealthcaregroup.
Thank you,
Irina Gorovaya, RN BSN, MBA
Amity Healthcare Group, LLC
Home Health Consulting, Education and Outsourcing Services
720-353-7249 (cell) 303-690-2749 (office) 720-398-6200 (fax)
www.amityhealthcaregroup.com


Confidentiality Notice:
The information contained in this message is privileged and confidential information intended for the use of the individual or entity named above.Copyright © 2022 Amity Healthcare Group, All rights reserved.
You are receiving this email because you opted in at our website
Amity Healthcare Group
5600 S. Quebec St Suite 310-A
Greewood Village, CO 8011