Hello, everyone!
Here are some home health related updates for this week:
AMITY’S NEWS
SPECIAL NEW CLIENT OFFER FOR THE MOTNTH OF OCTOBER (JUST 2 WEEKS LEFT!): If you subscribe to both, Skill Competency Program and Ongoing Training/Continued Education Management Program, you will receive 50% discount off the skilled competencies competed in the month of October.
Don’t forget, Ongoing Training/Continued Education Management Program is only $3.00 per user per month!!!)
Next available CNA/HHA and Skilled Nursing Competency is Tuesday, October 20, 2020 and Thursday, October 22, 2020.
If you would like to register your Skilled Nurses and/or HHAs/CNAs for a competency, please follow the links below:
Skilled Nursing Competency: https://amityhealthcaregroup.com/services/nursing-competencies/
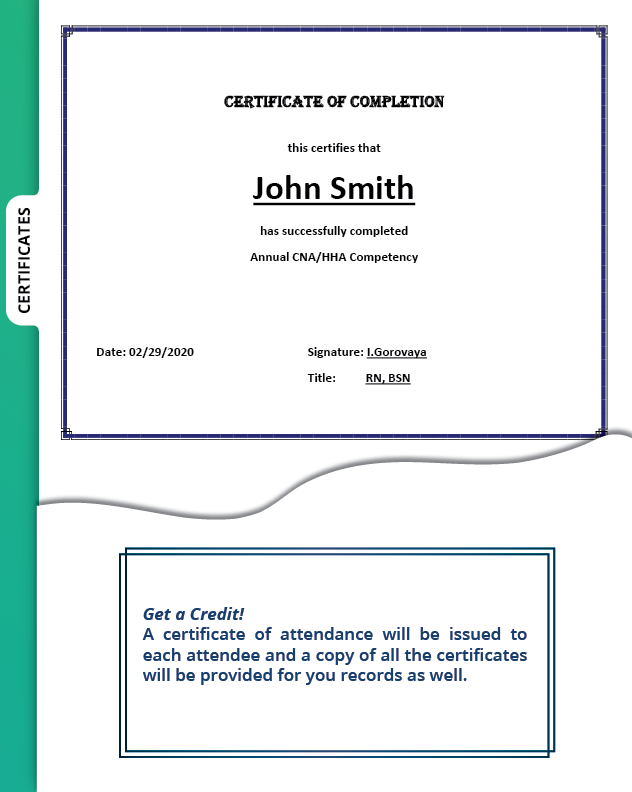
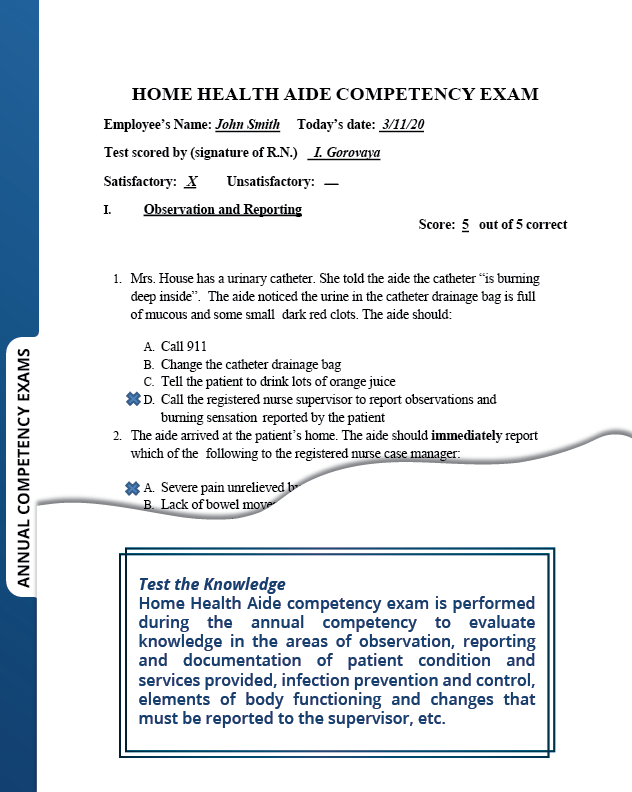
HHA/CNA Competency: https://amityhealthcaregroup.com/services/cna-hha-competency/
Let Amity Healthcare Group to assist you with staying compliant with competency and ongoing training/continued education requirements in a worry-free manner.
For more information, please call 303-690-2749 or email: ig@amityhealthcaregroup.com
NATIONAL NEWS
Extension of Public Health Emergency
The Public Health Emergency has been extended for another 90 days and is now set to expire on January 21, 2021. Extending the emergency declaration allows providers to continue to use waivers and flexibilities issued to assist in responding to the COVID-19 pandemic. Home Health and Hospice Waivers continue to be in effect until the end of the Public Health Emergency unless otherwise stated in the waiver.
CMS Announces New Repayment Terms for Medicare Loans (Accelerated and Advance Payment )Made to Providers During COVID-19
CMS announced amended terms for payments issued under the Accelerated and Advance Payment (AAP) Program. This Medicare loan program allows CMS to make advance payments to providers, which are typically used in emergency situations. Providers were required to make payments starting in August of this year, but under the Continuing Appropriations Act, 2021 and Other Extensions Act, repayment will now begin one year from the issuance date of each provider or supplier’s accelerated or advance payment.
After that first year, Medicare will automatically recoup 25% of Medicare payments otherwise owed to the provider or supplier for 11 months. At the end of the 11-month period, recoupment will increase to 50% for another 6 months. If the provider or supplier is unable to repay the total amount of the AAP during this time period (a total of 29 months), CMS will issue letters requiring repayment of any outstanding balance, subject to an interest rate of 4%.
For providers and suppliers who are experiencing financial hardships, it would be possible to request an Extended Repayment Schedule (ERS). An ERS is a debt installment payment plan that allows a provider or supplier to pay debts over the course of 3 years, or, up to 5 years in the case of extreme hardship. Providers and suppliers are encouraged to contact their MAC for information on how to request an ERS.
To allow even more flexibility in paying back the loans, the $175 billion issued in Provider Relief funds can be used towards repayment of these Medicare loans.
CMS will be communicating with each provider and supplier in the coming weeks as to the repayment terms and amounts owed as applicable for any accelerated or advance payment issued.
For additional information, please see attached Fact Sheet. You can also attend a CGS sponsored education event J15 Advanced & Accelerated Payment – Repayment Process on October 21, 2020 (please see registration information under Education Opportunities section of this email.
COLORADO NEWS
Provider Revalidation
As provider revalidation is on its way, please note that the deadlines for the next revalidation cycle will be in October 2020, based on previous enrollment approval dates. Providers will be contacted via email approximately 6 months prior to their revalidation deadline with further instructions. To check your revalidation due date, please go to https://www.colorado.gov/hcpf/revalidation and look for Provider Revalidation Dates Spreadsheet (it was last updated on 10/12/20)
In addition, you can also now find a new publication with step-by-step guide to the revalidation application process-Provider Revalidation Manual. The manual can be accessed at https://www.colorado.gov/pacific/sites/default/files/Provider%20Revalidation%20Manual%2010022020.pdf
Question of the Week
Last week we responded to the question “ If an Assisted Living Facility requires ALF staff to be tested for COVID on a weekly basis, can the ALF also require for home health agency to follow the same standards for the home health staff to be able to continue seeing patients in the ALF?” and determined that ALFs can require Home Health staff to follow the same procedures as ALF.
This week we had a follow up question:
Q: Is ALF required to provide COVID-19 testing for home health staff attending patients in ALF residence?
A: The ALF is not required to provide testing for contracted home care providers. The home care agency can set up their own free testing program through the state lab. The information on the state lab can be accessed at https://www.colorado.gov/pacific/cdphe/lab. Testing can also be arranged through a private lab at a cost.
EDUCATION OPPORTUNITIES
J15 Advanced & Accelerated Payment – Repayment Process
This event is geared towards agencies, facilities, and providers who received an Accelerated or Advanced Payments from Medicare due to the COVID-19 public health emergency. CGS will be offering information regarding the repayment process and what to expect.
October 21, 2020
12:30 p.m. – 13:30 p.m. Mountain Time
2:30 p.m. – 3:30 p.m. Eastern Time
Let’s RAP Home Health Providers
Join CGS for this educational forum that will surely answer some of your questions and provide a wealth of resources to reduce RAP anxiety related to upcoming changes to your Request for Anticipated Payments (RAPs). Pre-submitted questions may be submitted to J15_HHH_Education@cgsadmin.com
November 24, 2020
11:00 a.m. – 12:00 p.m. Mountain Time
1:00 p.m. – 2:00 p.m. Eastern Time
Please do not hesitate to reach out for any assistance or questions via email, phone or website at https://amityhealthcaregroup.com/resources/
If you wish to forward this email to your colleague or friend, please feel free to do so. If you received this message as a forward, we invite you to subscribe to our communications at https://amityhealthcaregroup.com/ (look for “Subscribe to Listserv” in the top corner). If you wish to unsubscribe from this email distribution list, please email to eg@amityhealthcaregroup.com
Thank you,
Irina Gorovaya, RN BSN, MBA
Amity Healthcare Group, LLC
Home Health Consulting, Education and Outsourcing Services
720-353-7249 (cell) 303-690-3749 (office) 720-398-6200 (fax)