Amity’s News!
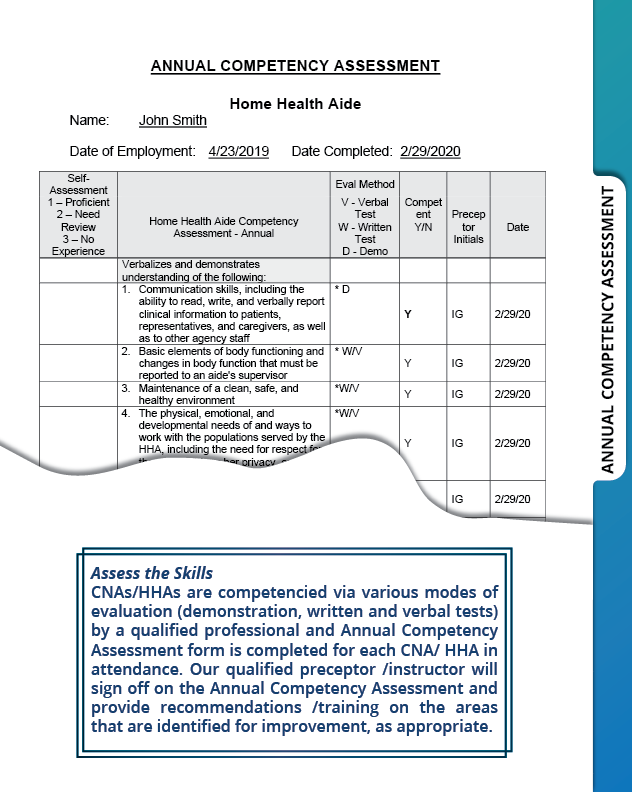
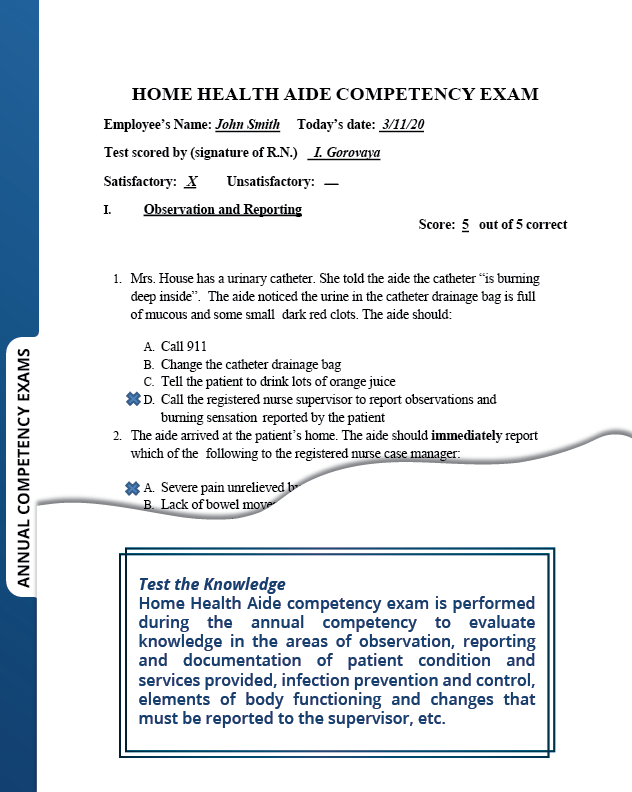
Learn about our ACHC and CHAP Recognized Products
CHAP verification for:
- Wound Management Program Policy and Procedure Manual
(this product could be extremely valuable for home health organizations specializing in wound care or agencies that would like to establish standardized approach/best wound care practices within the organization).

ACHC certification for:
- Home Health and Home Care admission packet
- Home Health and Home Care QAPI program
- Home Health Skilled Nursing Competency Program
We would like to ease some of your challenges and provide readily available solutions for your organizations.
For more information about our CHAP and ACHC certified products, please call 303-690-2749 or email ig@amityhealthcaregroup.com. Please also visit our website at https://amityhealthcaregroup.
OASIS -E Corner

Amity Healthcare Group is introducing a new rubric, “OASIS-E Corner”, to share the questions, challenging scenarios, and feedback that we come across working with our clients.
![]()
In this newsletter, we would like to share the following information with you:
N0415 High-Risk Drug Classes
There have been a lot of questions from clinicians in the field regarding this new OASIS-E item.
The key is determining if the patient is taking any prescribed medications in any of the drug classes specified in this item.
Do your staff members know how to identify drug classes
Some resources for determining drug classification include:
- Drugs.com https://www.drugs.com/drug-
classes.html - Global RPh Drug Reference https://globalrph.com/drugs/a
- Medline Plus https://medlineplus.gov/
druginformation.html
This item includes:
- All meds in drug class
- All settings (e.g., at home, in a hospital emergency room, at physician office or clinic)
- All routes
- All dosages
- Even if not taken on day of assessment
- Even if medication is not yet in the home or first dose has not been taken
- If part of the current drug regimen
Medications that have more than one therapeutic category and/or pharmacological classification should be coded in all categories/classifications assigned to the medication, regardless of how it is being used.
Combination medications should be coded in all categories/pharmacologic classes that constitute the combination.
NATIONAL NEWS
COVID-19 PHE Is Winding Down- What Home Health Agencies Need to Know

On January 30th, 2023, it was announced that the COVID-19 Public Health Emergency (PHE) will come to an end on May 11, 2023. Throughout the PHE various waivers and flexibilities were issued by CMS to allow needed response to the Pandemic. Some of these flexibilities have been made permanent, while others have been extended on multiple occasions, but will end on or after May 11.
In August 2022, CMS created a Roadmap including a provider-specific guidance for the end of the PHE to help guide providers towards returning to previous health and safety standards and practices. Since then, the Roadmap was updated, with the most recent update to Home Health guidance issued on February 1, 2023. Please note that it is possible that CMS will be making additional updates to the guidance in the near future. NAHC still has questions and concerns about expectations around provider responsibilities for some of the flexibilities and is awaiting a response from CMS.
From our experience, the most common flexibilities that providers continue to utilize are face-to-face encounter conducted via telehealth and OASIS completion and reporting. Both of these encounters are set to expire as follows:
- The required face-to-face encounter for home health can be conducted via telehealth(i.e., 2-way audio-video telecommunications technology that allows for real-time interaction between the physician/allowed practitioner and the patient) when the patient is at home. The face-to-face encounter can be conducted via telehealth irrespective of the COVID-19 PHE; however, the waiver will expire the first day after the 151st day following the end of the PHE.
- Reporting: CMS provided relief to HHAs on the timeframes related to OASIS transmission through the following 1) extending the five-day completion requirement for the comprehensive assessment to 30 days; and 2) waiving the 30-day OASIS submission requirement. CMS will end this waiver at the conclusion of the COVID-19 PHE.
The Provider Relief Fund Reporting Portal is Now Open for Reporting Period 4
Just a reminder that the Provider Relief Fund (PRF) Reporting Portal is now open for Reporting Period 4 (RP4). Providers who received a PRF (General or Targeted) and/or American Rescue Plan Rural payment(s), exceeding $10,000 in the aggregate, from July 1, 2021 to December 31, 2021 are required to report on their use of funds during RP4. The deadline to submit a report is March 31, 2023, at 11:59 p.m. ET.
Please remember that providers who experience one or more extenuating circumstances that prevent them from submitting a completed PRF Report by the deadline are offered a one-time opportunity to submit a Request to Report Late Due to Extenuating Circumstance. Review the Request to Report Late Due to Extenuating Circumstances webpage for more details in this process.
CMS Issues Proposals to Improve Exchange of Health Care Data and Prior Authorizations

The Centers for Medicare & Medicaid Services (CMS) issued a proposed rule to improve patient and provider access to health information and streamline processes related to prior authorization for medical items and services. CMS proposes to require certain payers to implement an electronic prior authorization process, shorten the time frames for certain payers to respond to prior authorization requests, and establish policies to make the prior authorization process more efficient and transparent.
The rule also proposes to require certain payers to implement standards that would enable data exchange from one payer to another payer when a patient changes payers or has concurrent coverage, which is expected to help ensure that complete patient records would be available throughout patient transitions between payers.
The proposal also includes requirements for certain payers to include a specific reason when denying requests, publicly report certain prior authorization metrics, and send decisions within 72 hours for expedited (i.e., urgent) requests and seven calendar days for standard (i.e., non-urgent) requests.
Proposed policies in this rule would also enable improved access to health data, supporting higher-quality care for patients with fewer disruptions.
These proposed requirements would generally apply to Medicare Advantage (MA) organizations, state Medicaid and Children’s Health Insurance Program (CHIP) agencies, Medicaid managed care plans, CHIP managed care entities, and Qualified Health Plan (QHP) issuers on the Federally-facilitated Exchanges (FFEs).
Most of the implementation dates for the proposals included in the proposed rule would begin in 2026. CMS believes a three year timeline would be sufficient to recruit and train staff, update or build the APIs, and update operational procedures.
HHVBP Resources

As you continue to navigate HHVBP, please remember to use Expanded HHVBP model resources. To provide home health agencies (HHAs) with a review of what to expect in the first performance year of the expanded HHVBP Model and highlight the resources provided during the pre-implementation year, the HHVBP Technical Assistance (TA) team created an on-demand video and downloadable resource, “First Performance Year Quick Guide”. It is now available on the Expanded HHVBP Model webpage under Quality Improvement.
Home Health Changes for Disaster Claims and Certain Adjustments – click here
CMS issued a Change Request (CR) Number: CR13020 with an effective date of 7/1/23 as a reminder to home health providers in conjunction to Revisions to Processing of Home Health Disaster Related Claims and Contractor-Initiated Adjustments.

This Change Request was issued due to the fact that HH&H MACs reported that HHAs submitted claims with condition code DR (indicating disaster related) during the COVID-19 PHE. However, no waiver of OASIS reporting has occurred during the current PHE, so condition code DR isn’t needed on these claims.
Make sure your staff knows:
- Only use condition code DR on disaster-related claims when Outcome and Assessment Information Set (OASIS) is waived
- No waiver of OASIS occurred for the current COVID-19 Public Health Emergency (PHE)
COLORADO NEWS
News from the Colorado Joint Budget Committee

Home Health providers have been awaiting for rates increase for some time now. Just to give you a little update, please note that at the end of January, Colorado Joint Budget Committee recommended a 3% across-the-board increase in HCPF provider rates, including for home health and private-duty nursing. This recommendation is good news as there is a potential for a bigger increase over the initial request from the Governor Polis administration for a half-percent across-the-board increase to most HCPF provider rates.
The provider rate increase, however, doesn’t apply to other so-called “targeted” rate increases being sought by the Home Care and Hospice Association of Colorado. Those discussions are ongoing and are considered separately during the HCPF figure-setting. So, the total funding picture for home health, home care and hospice remains incomplete.
To help advocate for higher reimbursement rates, sign up for HHAC’s legislative ambassador program: https://docs.google.com/forms/
Please also see Action Alert from Home Care and Hospice Association of Colorado below:
Action Alert: HHAC Needs Your Help Advocating for Rate Increases
To Colorado home care agencies –
Medicaid reimbursement rates will soon be set by the Legislature for home care in Colorado – and we need your help!
Please email your state legislators today to urge their support for important rate increase requests! Rates will be set by the Joint Budget Committee at the beginning of March, so there is no time to lose. The Colorado Home Care and Hospice Association of Colorado is requesting much-needed rate increases this year for home health, private duty nursing (PDN) and Home and Community Based Services (HCBS).
Here’s how to contact your legislators:
- Enter your zip code here to find your state representative and state senator, and their email addresses.
- Use the email template below to draft an email for your state legislators. We encourage you to personalize the email(s) and share how your agency and the communities you serve would benefit from increased Medicaid reimbursement rates. The more compelling and detailed your story, the more of an impact it will make.
- Be sure to replace all highlighted wording before your email is sent.
- Please CC or BCC protectcohomecare@gmail.
com.
Thank you for taking action on this today. Your voice can help build support for these important rate increases, before it’s too late.
HHAC Advocacy Team
******************************
Dear ***LEGISLATOR TITLE (Sen. or Rep.) + LAST NAME***,
My name is ***Your Name*** and I live in ***City/Town***. I am reaching out today about important budget requests this session that will impact services in your district. I would greatly appreciate your help and support in making sure these requests are included in the final budget bill passed by the Legislature.
Before I get into the specifics, I want to share with you why this issue is important to your district. ***Share your agency’s story and why adequate Medicaid reimbursement rates are essential. Use facts/figures and specific examples where possible. Make references to local communities to help reinforce your connection with the legislator’s district.***
That is why I am asking for your support for much-needed Medicaid rate increases for home care and personal care services in Colorado:
- Home Health Program: Please bring physical therapy and occupational therapy rates up to the same rate as speech therapy. This would be a $2.79 million impact to the state’s general fund.
- Private Duty Nursing (PDN) program: Please provide $20/hour increases for both Private Duty Nursing (PDN) RN and LPN rates. This would be a $17.4 million impact to the state’s general fund.
- Home and Community Based Services (HCBS): Please provide an 8.9% increase for HCBS personal care and homemaker services for both Denver and non-Denver rates to match inflation. This would be a $19.4 million impact to the state’s general fund and is $5.3 million more than what was included in the governor’s proposed budget. Please also extend the targeted rate increases for HCBS for January 1, 2023 – June 30, 2023 to match minimum wage increases that started Jan. 1 both inside Denver County and outside Denver County. The extension would have a $3.72 million impact on the state’s general fund.
I am also providing a link here to a handout from the Home Care and Hospice Association of Colorado that provides additional information about the value of these programs, not only for the state’s Medicaid population, but also for the taxpayers who fund these services.
Can I count on your support for these budget requests this year?
Please let me know. I am also happy to answer any questions you may have, or to find a time to meet and discuss this important issue if your schedule allows.
Thank you for your time, and for your service to our community.
Sincerely,
***Your Name***
**Agency name,** providing services in **list service area**
Private Duty Nursing Provider Update

A temporary administrative approval process for Private Duty Nursing (PDN) Prior Authorization Requests (PARs) was initially announced to be effective until December 31, 2022 and subsequently extended till February 28, 2023 has now been extended through April 2, 2023.
Please note that this is an administrative approval process not a pause. Providers still need to submit all necessary documentation to Kepro.
Amity’s newsletters will be archived on Amity’s Healthcare Group website at https://amityhealthcaregroup.
If you wish to forward this email to your colleague or friend, please feel free to do so. If you received this message as a forward, we invite you to subscribe to our communications at https://amityhealthcaregroup.
Thank you,
Irina Gorovaya, RN BSN, MBA
Amity Healthcare Group, LLC
Home Health Consulting, Education and Outsourcing Services
720-353-7249 (cell) 303-690-2749 (office) 720-398-6200 (fax)
www.amityhealthcaregroup.com






Confidentiality Notice:
The information contained in this message is privileged and confidential information intended for the use of the individual or entity named above.Copyright © 2022 Amity Healthcare Group, All rights reserved.
You are receiving this email because you opted in at our website
Amity Healthcare Group
5600 S. Quebec St Suite 310-A
Greewood Village, CO 8011