Amity’s News!
Learn about our ACHC and CHAP Recognized Products
CHAP verification for:
- Wound Management Program Policy and Procedure Manual

ACHC certification for:
- Home Health and Home Care admission packet
- Home Health and Home Care QAPI program
- Home Health Skilled Nursing Competency Program
We would like to ease some of your challenges and provide readily available solutions for your organizations.![]()
ORDER YOUR COPY TODAY!
For more information about our CHAP and ACHC certified products, please call 303-690-2749 or email ig@amityhealthcaregroup.com. Please also visit our website at https://amityhealthcaregroup.
OASIS -E Corner

In this newsletter, we would like to share the following information with you:
I) AV Fistula/AV Grafts Guidance
Per January 2023 CMS Quarterly OASIS Q&As, A-V fistula does not meet the definition of IV access for OASIS-E item O0110 O1. The guidance states “if there is not a current IV access in place at the time of assessment, and no other treatments, programs, or procedures listed in O0110 apply to the patient then code O0110 Z – None of the above.”
As a reminder, per OASIS guidance for OASIS item M1340, AV fistulas or grafts are considered surgical wounds once it is surgically created and as long as it is present in the patient’s body. For OASIS item M1342 for AV fistulas or grafts, enter response 0 – Newly epithelialized when the insertion site is healed and without signs and symptoms of infection.
II) Item D00150- Patient Mood Interview Guidance
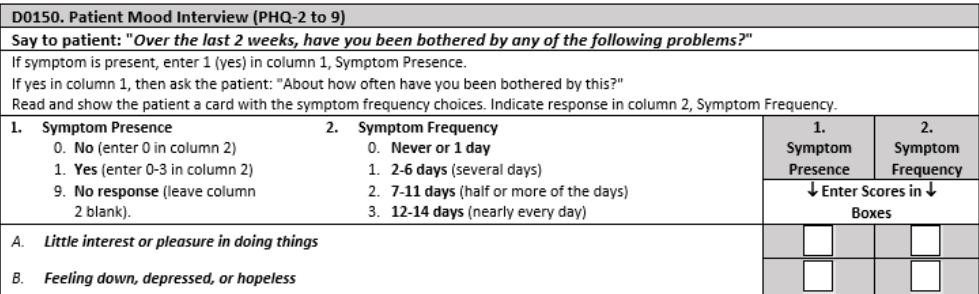
Tips:
- If the patient was unable or chose not to respond, clinician would enter code 9-No response in Column 1 and leave blank (or skip) Column 2.
- If the patient is rarely/never understood verbally, in writing, or using another method, clinician would enter code 9-No response in D0150 A1 and D0150 B1 and leave D0150 A2 and D0150B2 blank.
- If both D0150A1 and D0150B1 are coded 9-No response, leave D0150A2 and D0150B2 blank, then end the PHQ-2 and skip D0160, Total Severity Score.
NATIONAL NEWS
COVID-19 PHE Is Winding Down- What Home Health Agencies Need to Know

In our February 17th newsletter, we presented information related to guidance for home health providers pertaining to winding down of the PHE flexibilities and waivers in the light of the upcoming discontinuation of the PHE on May 11, 2023. That guidance was issued on February 1, 2023. Since then, CMS has issued an updated guidance on February 23, 2023.
Although majority of the guidance remains the same, there are several updates that will effect home health providers, including the following:
Face-to- Face Encounter:
One of the PHE flexibilities indicated that the required face-to-face encounter for home health can be conducted via telehealth (i.e., 2-way audio-video telecommunications technology that allows for real-time interaction between the physician/allowed practitioner and the patient) when the patient is at home. The face-to-face encounter can be conducted via telehealth irrespective of the COVID-19 PHE;
The original guidance indicated that the waiver would expire the first day after the 151st day following the end of the PHE. However, February 23rd guidance states the following:
After the PHE ends, the Consolidated Appropriations Act, 2023 provides for an extension for the flexibility to allow the home to be an originating site through December 31, 2024.
CMS Open Door Forum Updates

If you missed CMS Home Health and Hospice Open Door Forum that was held on February 23, 2023, here is the summary of the last week’s call:
Home Health Consumer Assessment of Healthcare Providers and Systems (HHCAHPS).
CMS reminded home health providers that home health agencies that are eligible for an exemption from participating in the HHCAHPS Survey for the CY 2024 (providers that served 59 or fewer survey eligible patients between April 1, 2021, and March 31, 2022.) must submit the exemption forms by March 31, 2023. The exemption forms may be located on the HHCAHPs website. CMS noted that the exemption applies only to the patient census during the year that qualified the agency for the exemption. If the agency’s census fluctuates during the reporting year, HHCAHPS participation is still required. CMS recommended HHAs contact the HHCAHPS contractor at hhcahps@rti.org or call 1-866-354-0985 for any questions regarding participation requirements.
Expanded Home Health Value Based Purchasing (HHVBP) Program
CMS reminded home health providers of a brief survey on the Expanded HHVBP model webpage requesting feedback on the home health agency’s experience with the expanded HHVBP Model resources and topics for future resources. The survey will close on March 31, 2023.
Please also take a moment to review FAQs for the month of February that address the transition to OASIS-E and its impact on the HHVPB.
CMS encouraged all home health providers to review your Pre-Implementation Performance Reports (PIPRs) that show home health agencies how their performance compares to other organizations in the assigned volume-based cohort, including statistics describing the distribution of performance scores. Last PIPR report was issued January 2023 and the next report will be available again April 2023. The reports are available through the IQIES. CMS reported that only about 20% of HHAs have downloaded their PIPRs so far.
Home Health Quality Reporting Program (HHQRP)
CMS announced updated resources on the Home Health Quality Measure webpage related to transition to OASIS-E, including updates to the quality measures tables and the risk adjustment model. These updates are applied to starts of care and resumptions of care assessments with M0090 dates on or after January 1, 2023. CMS announced that the following quality measures have revised calculations that will exclude discharges to hospice.
- Improvement in Ambulation – Locomotion
- Improvement in Bed Transferring
- Improvement in Toilet Transfer
- Improvement in Bathing
- Improvement in Management of Oral Medications
- Improvement in Dyspnea
- Improvement in Upper Body Dressing
- Improvement in Lower Body Dressing
- Improvement in Bowel incontinence
- Improvement in Confusion Frequency
- Discharge to Community
A revised HHQRP Quality Measures User’s Manual has been released and can be found on the Home Health Quality Measure webpage.
CMS Webinar on CY 2023 Home Health Final Rule

Join CMS experts as they provide an overview of several provisions from the CY 2023 HH PPS final rule related to behavior changes, the construction of 60-day episodes, and payment rate development for CY 2023. Visit the Home Health Patient-Driven Groupings Model webpage for more information and materials.
The webinar is scheduled for Wednesday, March 29 from 1:30-3:00 PM ET. A registration link is on the CMS Home Health Center webpage.
COLORADO NEWS
Timely Claims Submission
The Colorado Department of Health Care Policy and Financing is reminding providers of the fact that providers are required to submit an initial claim within 365 days, even if the result is a denial. Providers must also resubmit claims every 60 days after the initial timely filing period (365 days from the date of service [DOS]) to keep the claim within the timely filing period. The previous Internal Control Number (ICN) must be referenced on the claim if the claim is over 365 days. Waiting for prior authorization or correspondence from the Department of Health Care Policy & Financing (the Department) or the fiscal agent is not an acceptable reason for late filing. Phone calls and other correspondence are not proof of timely filing. The claim must be submitted, even if the result is a denial.
Visit the Timely Filing Frequently Asked Questions web page for more information.

Advocate for Rate Increase
If you have not done so yet, please help Home Care and Hospice Association of Colorado to advocate for rate increase for home health and home care.
Please email your state legislators by March 3, 2023 as noted below.
Action Alert: HHAC Needs Your Help Advocating for Rate Increases
To Colorado home care agencies –
Medicaid reimbursement rates will soon be set by the Legislature for home care in Colorado – and we need your help!
Please email your state legislators today to urge their support for important rate increase requests! Rates will be set by the Joint Budget Committee at the beginning of March, so there is no time to lose. The Colorado Home Care and Hospice Association of Colorado is requesting much-needed rate increases this year for home health, private duty nursing (PDN) and Home and Community Based Services (HCBS).
Here’s how to contact your legislators:
- Enter your zip code here to find your state representative and state senator, and their email addresses.
- Use the email template below to draft an email for your state legislators. We encourage you to personalize the email(s) and share how your agency and the communities you serve would benefit from increased Medicaid reimbursement rates. The more compelling and detailed your story, the more of an impact it will make.
- Be sure to replace all highlighted wording before your email is sent.
- Please CC or BCC protectcohomecare@gmail.
com.
Thank you for taking action on this today. Your voice can help build support for these important rate increases, before it’s too late.
HHAC Advocacy Team
******************************
Dear ***LEGISLATOR TITLE (Sen. or Rep.) + LAST NAME***,
My name is ***Your Name*** and I live in ***City/Town***. I am reaching out today about important budget requests this session that will impact services in your district. I would greatly appreciate your help and support in making sure these requests are included in the final budget bill passed by the Legislature.
Before I get into the specifics, I want to share with you why this issue is important to your district. ***Share your agency’s story and why adequate Medicaid reimbursement rates are essential. Use facts/figures and specific examples where possible. Make references to local communities to help reinforce your connection with the legislator’s district.***
That is why I am asking for your support for much-needed Medicaid rate increases for home care and personal care services in Colorado:
- Home Health Program: Please bring physical therapy and occupational therapy rates up to the same rate as speech therapy. This would be a $2.79 million impact to the state’s general fund.
- Private Duty Nursing (PDN) program: Please provide $20/hour increases for both Private Duty Nursing (PDN) RN and LPN rates. This would be a $17.4 million impact to the state’s general fund.
- Home and Community Based Services (HCBS): Please provide an 8.9% increase for HCBS personal care and homemaker services for both Denver and non-Denver rates to match inflation. This would be a $19.4 million impact to the state’s general fund and is $5.3 million more than what was included in the governor’s proposed budget. Please also extend the targeted rate increases for HCBS for January 1, 2023 – June 30, 2023 to match minimum wage increases that started Jan. 1 both inside Denver County and outside Denver County. The extension would have a $3.72 million impact on the state’s general fund.
I am also providing a link here to a handout from the Home Care and Hospice Association of Colorado that provides additional information about the value of these programs, not only for the state’s Medicaid population, but also for the taxpayers who fund these services.
Can I count on your support for these budget requests this year?
Please let me know. I am also happy to answer any questions you may have, or to find a time to meet and discuss this important issue if your schedule allows.
Thank you for your time, and for your service to our community.
Sincerely,
***Your Name***
**Agency name,** providing services in **list service area**
Private Duty Nursing Provider Update

A temporary administrative approval process for Private Duty Nursing (PDN) Prior Authorization Requests (PARs) was initially announced to be effective until December 31, 2022 and subsequently extended till February 28, 2023 has now been extended through April 2, 2023.
Please note that this is an administrative approval process not a pause. Providers still need to submit all necessary documentation to Kepro.
Amity’s newsletters will be archived on Amity’s Healthcare Group website at https://amityhealthcaregroup.
If you wish to forward this email to your colleague or friend, please feel free to do so. If you received this message as a forward, we invite you to subscribe to our communications at https://amityhealthcaregroup.
Thank you,
Irina Gorovaya, RN BSN, MBA
Amity Healthcare Group, LLC
Home Health Consulting, Education and Outsourcing Services
720-353-7249 (cell) 303-690-2749 (office) 720-398-6200 (fax)
www.amityhealthcaregroup.com







Confidentiality Notice:
The information contained in this message is privileged and confidential information intended for the use of the individual or entity named above.Copyright © 2022 Amity Healthcare Group, All rights reserved.
You are receiving this email because you opted in at our website
Amity Healthcare Group
5600 S. Quebec St Suite 310-A
Greewood Village, CO 8011

